At 28 weeks and five days into my first pregnancy, during a follow-up prenatal appointment, my blood pressure spiked. I was brought to labor and delivery triage and, shortly after, I was diagnosed with severe preeclampsia. What followed was an anxious 31-day hospitalization in the antepartum unit and then an exhausting but joyous four-day postpartum stay.
Hospitalizations have known problems, including risk of infection, risk of blood clots from inactivity, and the stress of your life coming to a standstill. As an innovation consultant whose job is to help clients develop new or reimagine existing products, services, and experiences, I couldn’t help thinking about the hospitalization experience during my stay. But I saw that a properly redesigned hospital experience would need to range beyond the limits of mere healthcare. Fortunately, because my organization works on a variety of projects across multiple industries, it is second nature to apply insights and draw inspiration from a variety of different systems.
While I’m grateful for the wonderful care I received, my hospitalization taught me there could be meaningful, non-clinical ways to understand and improve the hospital experience for both patients and providers.
Sleep, Interrupted: The Challenge of Nighttime Vitals Checks
Patients sleep terribly in hospitals. The strange noises, the lack of privacy, and the unfamiliar setting can make it nearly impossible to get a very necessary good night’s rest. During my hospitalization, I had my vitals checked at a minimum every four hours. On bad days, it could be as frequent as every 15 minutes. Every night during my hospitalization, I would be woken up one-to-two times to have vitals checked.
How might we capture patient vitals at night without requiring them to wake up?
Solutions could range from helping night nurses recognize and utilize the time when a patient may already be awake to managing by exception through wearables and smart objects. EPAM Continuum recently had Preventric’s Dr. Ali, Preventric’s Chief Medical Officer on The Resonance Test. Their wearable monitors blood pressure while the wearer is asleep. Teslasuit offers a full-body haptic garment that has been used to monitor and collect biometric parameters in patients. We spoke with Teslasuit’s CEO and head of research to discuss the possibilities.
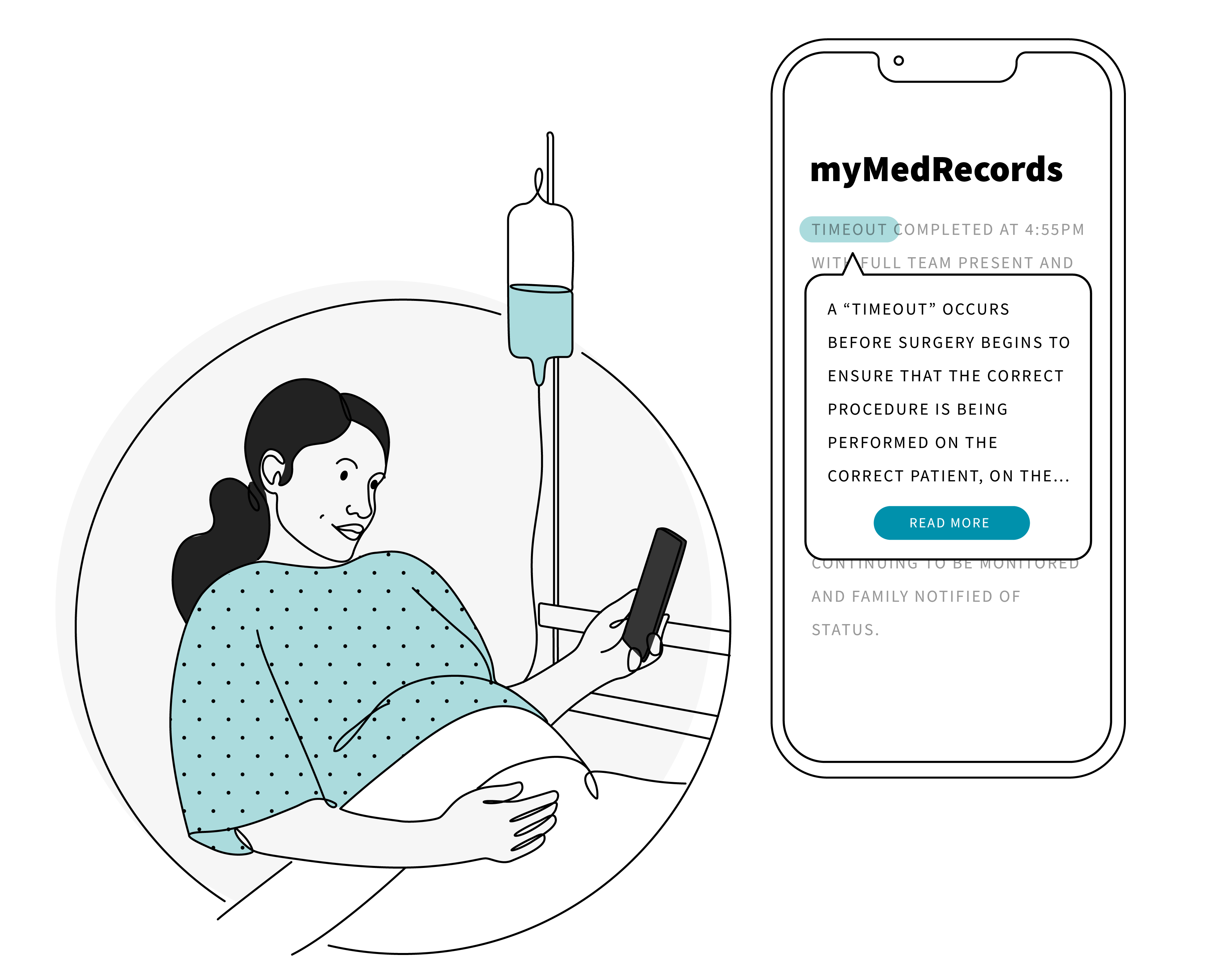
Misunderstanding Medical Records
With digital medical record apps becoming ubiquitous, patients have almost instant access to their medical records. With little to do and being bored most of the time, receiving notifications of new test results or seeing my medical chart being updated became a new form of daily entertainment. Reading medical notes is like reading a new language. It involves, much to a doctor’s chagrin, Googling abbreviations, acronyms, and terminology. Sometimes words that seem to be layman’s terms may have different medical meanings. As a patient, this lack of understanding the language being used could a lead patient to feeling they are being ignored, misunderstood, or dismissed. However, doctors need to maintain medical accuracy of medical records to ensure they aren’t jeopardizing their patients’ health.
How might we help patients better understand what doctors are writing in order to reduce confusion and frustration?
We might apply the lessons of our project with Southwest Airlines to the hospitalization experience: Improve communications by translating terms into clear human language. Solutions could range from offering plain language definitions of terms to applying machine learning that “translate” doctor lingo.

What to Expect When You’re Expecting a Doctor
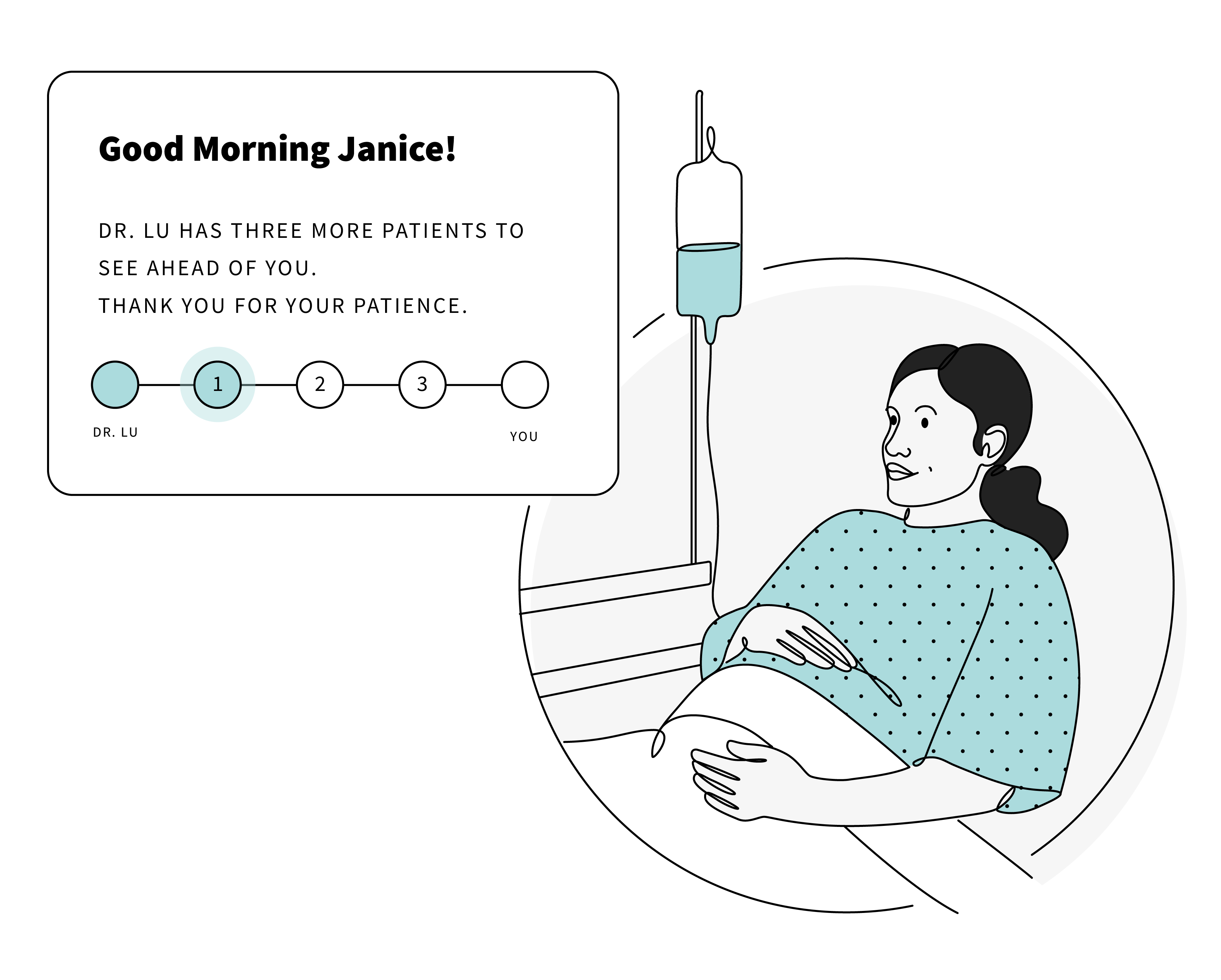
Patients want to know that their doctor, specifically the attending on call, is paying attention to their case. For patients, the feedback for this is more facetime with the attending. However, attendings manage their time by “managing by exception.” More facetime with the attending typically means something is wrong. On my good days, I would only see the attending during morning rounds to discuss the plan for the day. On bad days, I saw the attending outside of this time, either because my blood pressure had spiked and needed to be controlled or a serious medical discussion needed to occur. As a patient, hindsight is 20/20. During your stay, not seeing the attending can lead to concern that your case isn’t being monitored and worse, if something is wrong, no one will notice. This leads to the broader issue of unclear expectations during a hospital stay. While patients are given a general sense of what will happen, the who, when, and sometimes why are out of the patients control and very rarely communicated with a set timeline. Understandably, this is because hospital staff are prioritizing their time with the less stable patients. However, these unclear expectations may lead to anxiety and impatience.
Hospital staff are already overburdened and, at times, understaffed. The goal shouldn’t be to sacrifice hospital staff experience (and priorities) for the ideal patient experience. Instead, innovative ideas should find ways to utilize already existing electronic information to both reduce the workload of hospital staff and improve how information is communicated to the patient.
How do we assure patients that they are being monitored and cared for without them constantly wanting to see the attending?
Utilizing the smartphones patients have and the TVs throughout patient rooms, solutions could be anything from sharing out how the medical team is monitoring the patient to visualizing, even roughly, a patient’s schedule for the day. Additionally, hospitals could borrow our approach to the Future of First Response by mapping where healthcare providers are in the building to give patients a better sense of when they would see a doctor, nurse, or tech.

Fewer Pain Points, Happier Hospital Experience
As a new parent to a happy and healthy son, I look back on my hospital stay as a surreal but formative experience that I hope no one else ever must go through. However, the reality is that life happens to all of us as our families grow and age. We become alpha daughters and caregivers, and occasionally, patients ourselves. With the stress and complications that come with this, it becomes even more important that we find opportunities and solutions to alleviate the mental stresses and burdens patients face to ensure a quick recovery.
Images by Natasha Polozenko




